A clear guide to LDL, HDL, triglycerides, risk factors, testing, and practical ways to improve heart health.
Introduction
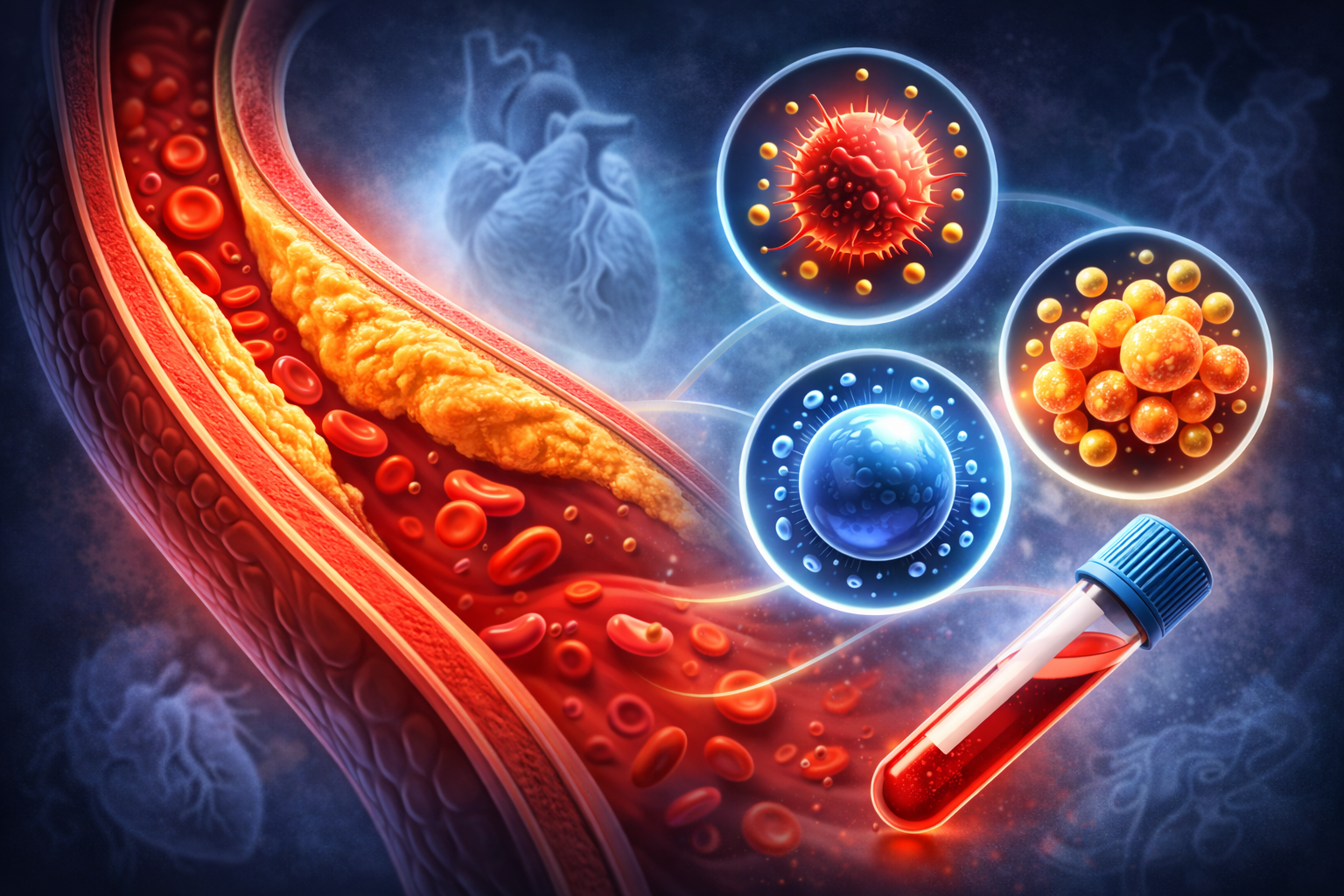
“Cholesterol problems” usually means your blood test shows high LDL (often called “bad” cholesterol), low HDL (“good” cholesterol), high triglycerides, or a combination of these. These numbers matter because they can increase the risk of heart disease and stroke over time.
The good news: many people can improve their cholesterol profile with lifestyle changes, and when needed, medication can reduce risk even further. This article explains what cholesterol is, what the lab numbers mean, why cholesterol problems happen, and what you can do step by step.
What Is Cholesterol?
Cholesterol is a waxy substance your body uses to build cells and make hormones. Your liver makes cholesterol, and you also get some from food. Cholesterol travels in your blood attached to proteins called lipoproteins.
The most common cholesterol-related tests include:
- LDL (Low-Density Lipoprotein): Often called “bad” cholesterol because it can contribute to plaque buildup in arteries.
- HDL (High-Density Lipoprotein): Often called “good” cholesterol because it helps move cholesterol away from arteries.
- Triglycerides: A type of blood fat linked to calories and energy storage; high levels can increase risk.
- Total cholesterol: A combined number (less informative alone than the individual parts).
- Non-HDL cholesterol: Total cholesterol minus HDL; a useful “all bad particles” estimate.
Why Cholesterol Problems Matter
When LDL and other “atherogenic” particles are high, they can contribute to plaque buildup in artery walls. Over time, this can narrow arteries and raise the risk of:
- Heart attack
- Stroke
- Peripheral artery disease
Cholesterol problems usually develop silently—many people feel normal until a serious event happens—so prevention matters.
Common Cholesterol Patterns
High LDL
Often linked to genetics, diet patterns, and overall risk factors. Reducing LDL is a major target for risk reduction.
Low HDL
Often associated with inactivity, smoking, excess body weight, and insulin resistance. Focus is usually on overall lifestyle rather than “raising HDL” alone.
High Triglycerides
Often related to excess calories, sugary drinks, refined carbs, alcohol, uncontrolled diabetes, or certain medications.
Mixed Dyslipidemia
A mix of high LDL + high triglycerides + low HDL, commonly seen with metabolic syndrome and insulin resistance.
What Causes Cholesterol Problems?
Cholesterol levels come from a mix of genetics and lifestyle. Common contributors include:
Diet Patterns
- High saturated fat intake (certain meats, full-fat dairy, some processed foods)
- High trans fats (less common now, but still in some fried/processed items)
- High added sugars and refined carbs (raise triglycerides)
- Low fiber intake
Body Weight and Inactivity
- Excess body fat can worsen LDL and triglycerides
- Low activity can reduce HDL and worsen insulin resistance
Genetics
- Family history of high cholesterol
- Familial hypercholesterolemia (very high LDL from a young age)
Medical Conditions
- Diabetes or insulin resistance
- Hypothyroidism
- Kidney disease
- Liver conditions
Alcohol and Smoking
- Alcohol can increase triglycerides (especially at higher intake)
- Smoking can lower HDL and damage blood vessels
Medications
- Some steroids, diuretics, and other medications can affect lipids
- Always discuss changes with your clinician before stopping any medicine
Understanding Your Lab Results (General Concepts)
Cholesterol goals differ depending on your overall cardiovascular risk. Your clinician may look beyond “normal ranges” and aim for more aggressive LDL lowering if you have diabetes, high blood pressure, smoking history, kidney disease, a strong family history, or known heart disease.
How to Improve Cholesterol: What Works Best
The most effective approach is usually a combination of nutrition, activity, weight management (if needed), and addressing medical conditions. Below are practical strategies.
1) Improve Your Diet (Heart-Friendly Patterns)
You don’t need a perfect diet—just a sustainable pattern. A heart-friendly approach often includes:
- More fiber: vegetables, fruit, beans, lentils, oats, barley, whole grains.
- Healthy fats: olive oil, nuts, seeds, avocado, fatty fish (salmon, sardines).
- Lean proteins: fish, poultry, beans, tofu, low-fat dairy (as tolerated).
- Less processed food: fewer fried items, sugary snacks, and packaged ultra-processed meals.
- Less added sugar: especially sugary drinks and desserts (helps triglycerides).
2) Reduce Saturated and Trans Fats
Saturated fats can raise LDL in many people. You don’t have to remove them completely—just reduce and replace them with healthier fats.
- Reduce: fatty red meats, processed meats, butter, some baked goods.
- Replace with: olive oil, nuts, seeds, fish, beans, and lean proteins.
3) Choose Smarter Carbs (Especially for High Triglycerides)
- Favor whole grains over refined grains (white bread, pastries).
- Limit sugar-sweetened drinks and frequent desserts.
- Balance carbs with protein and fiber to prevent spikes.
4) Move Your Body Consistently
Activity improves triglycerides, supports HDL, helps blood pressure, and improves insulin sensitivity. You don’t need to “go hard”—consistency matters most.
- Start simple: brisk walking 20–30 minutes most days.
- Add strength training: 2 days per week if possible.
- Daily movement: even short walks after meals can help metabolism.
5) Manage Weight (If Needed)
Even modest weight loss in people with excess body weight can improve LDL, triglycerides, and insulin resistance. Focus on sustainable habits rather than extreme dieting.
6) Improve Sleep and Stress Habits
Poor sleep and chronic stress can contribute to unhealthy eating patterns and metabolic changes. A stable routine helps your overall risk profile.
7) Limit Alcohol (Especially if Triglycerides Are High)
Alcohol can increase triglycerides for some people. If your triglycerides are high, consider reducing or stopping alcohol and re-checking labs after a few months.
When Medication Might Be Needed
Lifestyle changes are the foundation, but some people need medication—especially if LDL is very high, if there is a strong family history, or if someone has higher overall cardiovascular risk.
Common medication categories include cholesterol-lowering drugs that reduce LDL or triglycerides. Decisions are personalized and based on your risk, age, and lab results.
Warning Signs: When to Seek Urgent Care
High cholesterol itself usually does not cause symptoms. But heart attack or stroke symptoms require urgent care:
- Chest pressure/pain, shortness of breath, sweating, nausea (possible heart attack)
- Sudden weakness/numbness on one side, speech trouble, facial droop (possible stroke)
- Sudden severe headache, confusion, or vision changes
A Simple 8-Week Cholesterol Improvement Plan
- Week 1–2: Replace sugary drinks with water or unsweetened tea.
- Week 1–2: Add one high-fiber food daily (oats, beans, veggies).
- Week 3–4: Walk 20 minutes after dinner 4–5 days per week.
- Week 3–4: Swap butter/fatty meats more often for olive oil, fish, or beans.
- Week 5–6: Add 2 strength sessions per week (bodyweight is fine).
- Week 5–6: Plan snacks: fruit + nuts, yogurt, or hummus + veggies.
- Week 7–8: Review progress and keep the habits you can maintain long-term.
Quick Summary
- Cholesterol problems often involve high LDL, low HDL, high triglycerides, or a mix.
- They matter because they raise the risk of heart disease and stroke over time.
- The biggest lifestyle levers: fiber, healthier fats, fewer added sugars, consistent movement, weight management, and good sleep.
- Some people need medication due to genetics or higher overall risk—this can significantly reduce future risk.