A practical guide to digestion issues—what’s normal, what’s not, and when to get help.
Introduction
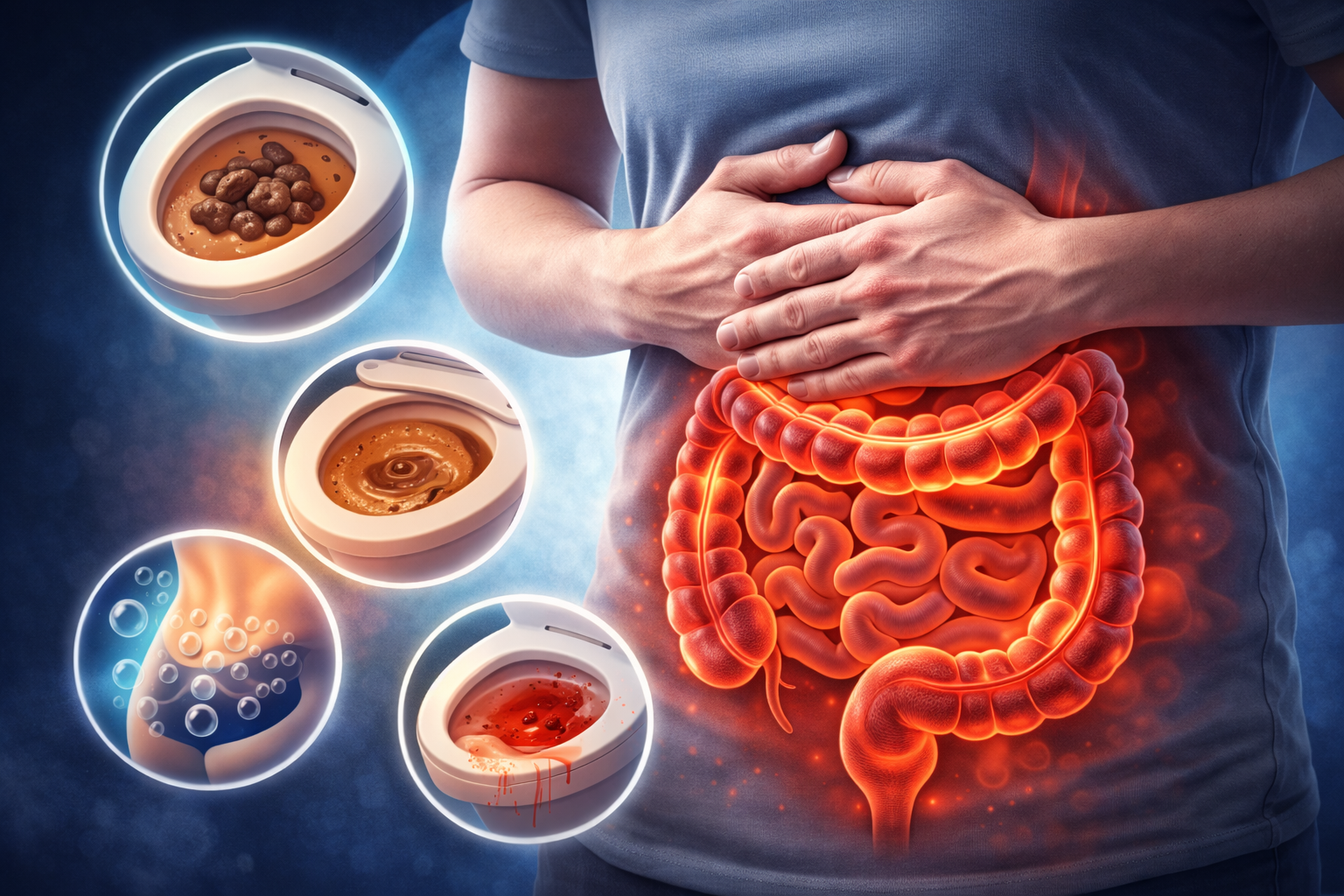
“Bowel problems” is a broad term that can include constipation, diarrhea, bloating, gas, abdominal pain, changes in stool appearance, urgency, or feeling like you can’t fully empty your bowels. Almost everyone experiences these issues at some point, and many are caused by food, stress, infections, dehydration, or changes in routine.
But sometimes bowel problems can be a sign of an underlying condition that needs medical attention. This article explains common bowel symptoms, likely causes, safe self-care strategies, and warning signs that mean you should contact a healthcare professional.
What’s “Normal” for Bowel Movements?
Normal bowel habits vary widely. Some people go 3 times per day; others go 3 times per week. What matters most is your personal normal—and whether anything has changed suddenly.
- Normal stool: soft, formed, easy to pass, not painful, no blood.
- Healthy frequency: can vary; consistency and comfort matter more than a specific number.
- Color: usually shades of brown. Some foods and medicines can change color temporarily.
Common Bowel Problems (And What They Often Mean)
1) Constipation
- Hard or dry stool
- Straining
- Going less often than usual
- Feeling “blocked”
Common triggers: low fiber, dehydration, inactivity, travel, certain meds, ignoring urge to go.
2) Diarrhea
- Loose or watery stool
- Urgency
- More frequent bowel movements
Common triggers: viral/bacterial infection, food intolerance, stress, antibiotics, too much caffeine or sugar alcohols.
3) Bloating & Gas
- Fullness, pressure, swelling feeling
- Excess gas, burping, passing gas
Common triggers: swallowing air, carbonated drinks, beans, dairy intolerance, constipation, IBS, stress.
4) Abdominal Pain or Cramping
- Crampy pain linked with bowel movements
- Pain with diarrhea or constipation
Common triggers: infection, food intolerance, constipation, IBS, inflammation, menstrual-related symptoms.
5) Urgency or “Can’t Hold It”
- Sudden need to go
- Fear of accidents
Common triggers: infection, IBS, inflammatory bowel disease, anxiety, certain foods (spicy/greasy).
6) Blood on Toilet Paper or in Stool
- Bright red blood with wiping
- Blood mixed with stool
Common triggers: hemorrhoids, anal fissures (small tears), but sometimes more serious causes.
Common Causes of Bowel Problems
Bowel symptoms can come from many sources. Here are some major categories:
Diet & Hydration
- Low fiber intake
- Not enough water
- High-fat or very processed foods
- Food intolerances (lactose, gluten sensitivity for some)
- Artificial sweeteners (sorbitol, mannitol)
Infections
- Viruses (“stomach flu”)
- Food poisoning
- Traveler’s diarrhea
Stress & Gut-Brain Connection
- Stress can speed up or slow down digestion
- Anxiety can increase urgency
- Poor sleep may worsen gut symptoms
Medications & Supplements
- Antibiotics (can cause diarrhea)
- Iron supplements (can cause constipation)
- Opioid pain meds (constipation)
- Some antacids and diabetes meds
Functional Disorders (Common)
- IBS (Irritable Bowel Syndrome): abdominal pain + bowel changes without structural disease
- Constipation-predominant, diarrhea-predominant, or mixed patterns
Inflammation or Structural Problems
- IBD (Crohn’s disease, ulcerative colitis)
- Diverticular disease
- Gallbladder issues
- More serious conditions (less common) depending on symptoms
Self-Care: What You Can Try at Home (Safe Basics)
If symptoms are mild and you don’t have warning signs, these steps can help many common bowel problems. Adjust slowly—your gut often needs time to adapt.
General “Gut Reset” Habits
- Hydrate: drink water regularly; dehydration often causes constipation and worsens cramps.
- Move daily: walking helps bowel movement and reduces bloating.
- Eat slowly: reduces swallowed air and gas.
- Keep a food/symptom log: helps identify triggers (dairy, spicy foods, greasy meals, etc.).
- Routine matters: regular meals and sleep support regular bowel movements.
Constipation: Practical Tips
- Add fiber slowly: fruits, vegetables, oats, beans, whole grains.
- Try prunes or kiwi: some people find them helpful.
- Don’t ignore the urge: delaying can worsen constipation.
- Use a “toilet posture”: knees higher than hips (a small footstool can help).
- Consider a fiber supplement: if diet is low in fiber (start small, increase slowly).
Diarrhea: Practical Tips
- Prevent dehydration: sip water, oral rehydration solutions, or broths.
- Eat gentle foods: rice, bananas, applesauce, toast, oatmeal, soup.
- Avoid irritants: alcohol, high-fat meals, lots of caffeine, very spicy foods.
- Watch for blood or fever: these can suggest infection that needs medical evaluation.
Bloating & Gas: Practical Tips
- Check constipation: constipation commonly causes bloating.
- Reduce carbonated drinks and chewing gum (swallowed air).
- Try smaller meals and eat slowly.
- Identify triggers: beans, dairy, onions, garlic, certain sweeteners.
- Gentle movement: walking after meals can reduce gas.
Hemorrhoids and Anal Fissures (Common Causes of Bright Red Blood)
Bright red blood on toilet paper is often caused by hemorrhoids (swollen veins) or fissures (tiny tears), especially with hard stool and straining.
- Prevent constipation: fiber + water + movement.
- Warm sitz baths: can reduce discomfort.
- Avoid heavy straining: take your time, and don’t force.
Warning Signs (Red Flags) — Get Medical Help
Seek medical care urgently if you have:
- Severe or worsening abdominal pain (especially with tenderness or guarding).
- Blood in stool that is heavy, persistent, or mixed with stool.
- Black, tarry stools (can suggest bleeding higher in the digestive tract).
- High fever or severe illness.
- Signs of dehydration (dizziness, confusion, very dark urine, fainting).
- Unexplained weight loss or loss of appetite.
- Persistent vomiting or inability to keep fluids down.
- New bowel changes that last weeks, especially after age 45–50 or with family history of colon cancer.
- Severe constipation with swelling and inability to pass gas (possible obstruction).
What to Expect at a Medical Visit
A clinician may ask about your symptoms, diet, medications, stress, and family history. Depending on your situation, they may recommend:
- Basic blood tests (for anemia, infection, inflammation).
- Stool tests (for infection or inflammation markers).
- Imaging (if pain is severe or obstruction is suspected).
- Endoscopy/colonoscopy (if there are red flags, bleeding, or persistent changes).
Prevention: Daily Habits for a Healthier Gut
- Eat more fiber: vegetables, fruit, beans, whole grains (increase slowly).
- Drink enough fluids: especially if increasing fiber.
- Move regularly: walking, cycling, light exercise supports bowel movement.
- Manage stress: relaxation, breathing, good sleep, and routines can help IBS-like symptoms.
- Limit ultra-processed foods: high in fat, low in fiber, often worsen gut issues.
Quick Summary
- Bowel problems are common and often triggered by diet, dehydration, stress, infections, or medications.
- Mild symptoms may improve with hydration, fiber, movement, and identifying food triggers.
- Watch for red flags like heavy bleeding, black stools, severe pain, fever, dehydration, or unexplained weight loss.
- If symptoms persist or worsen, a medical checkup can rule out serious causes and help you find the right treatment.